Overcoming Irritable Bowel Syndrome (IBS) Through Diet, Management, and Prevention

Discover how to manage and overcome Irritable Bowel Syndrome (IBS) through a diet modifications, stress management, and preventative measures
Uncovering Types of IBS
IBS with constipation
IBS that causes constipation makes people go to the bathroom less often, have trouble passing faeces, and feel like they haven't gotten rid of everything. Abdominal pain, bloating, and gas may accompany this type of IBS.
IBS with constipation is often caused by gut muscle issues. These digestive muscles contract and relax to transport food and waste. IBS-related constipation is caused by weak or sluggish muscular contractions.
Foods can also aggravate constipation-related IBS. These include processed, sugary, and fatty foods. IBS and constipation sufferers should keep a food diary to identify and prevent triggers.
Changes in lifestyle may also help with IBS constipation. Exercise, water, and a high-fiber diet are examples. Medication may help relieve symptoms.
IBS with diarrhoea
IBS with diarrhoea causes diarrhoea. Diarrhoea and IBS can cause frequent, loose faeces. Gas, bloating, and abdominal pain may occur.
Rapid contractions of the intestine can cause both pain and faster stool movement. This gives the intestine less time to absorb water from the digested matter, which leads to loose or watery stools.
Some patients develop IBS-D as a result of a previous intestinal infection. This is known as post-infectious IBS. It can last for weeks, months, or even years following a gut infection.
For some people with IBS-D, sensitivity or allergy to particular foods may also be a factor. Many patients experience symptoms after consuming specific food components, such as lactose or gluten. In these cases, avoiding foods containing those ingredients can improve symptoms. Unfortunately, routine allergy testing is not a reliable way to determine whether or not specific foods are causing IBS symptoms.
Some IBS patients have a more sensitive gut, and they experience more pain or discomfort from gas or intestinal contractions than the general population.
Recent research suggests that changes in the type or number of normal bacteria living in the gut may contribute to IBS-D symptoms.
Foods may also aggravate IBS by causing diarrhoea. These include processed sugary, and fatty foods. IBS patients with diarrhoea should keep a food diary to identify and prevent triggers.
Lifestyle changes may also help IBS with diarrhoea. Exercise, water, and a high-fibre diet are examples. Medication may help relieve symptoms.
Finally, while stress and anxiety are not thought to cause IBS-D, they can play a significant role in exacerbating the symptoms.
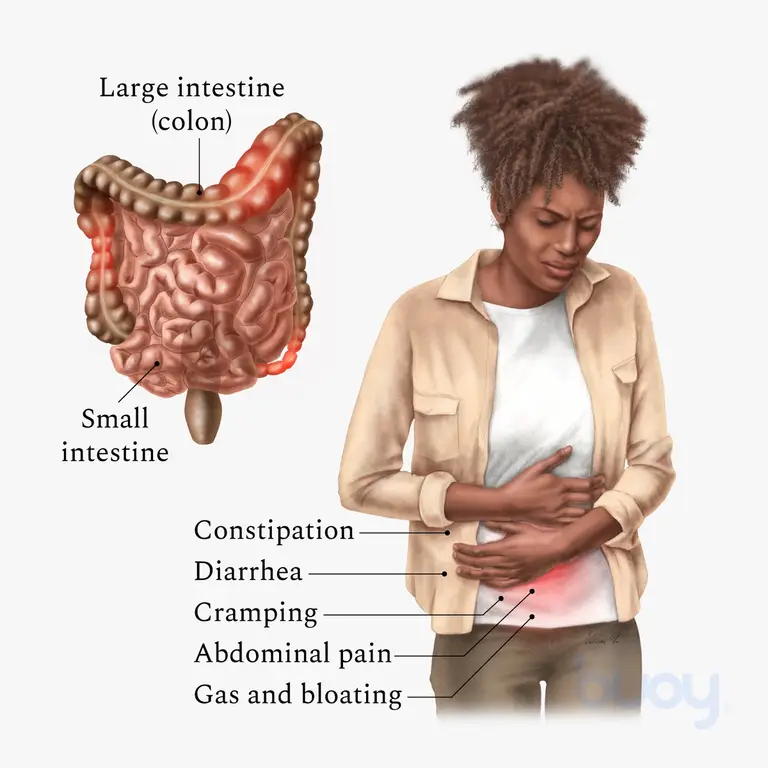
IBS-mixed
IBS mixed is a subtype of IBS in which people experience both constipation and diarrhoea. This subtype of IBS is also known as IBS-M (IBS with alternating bowel habits) or IBS-A (IBS with alternating symptoms). People with IBS-M may experience a fluctuation of symptoms, such as constipation one day and diarrhoea the next.
Foods to Avoid with Irritable Bowel Syndrome (IBS)
There is no definitive list of foods that trigger IBS symptoms, as they can vary from person to person. However, some common food triggers include:
1. High-FODMAP Foods: These are foods that are high in certain types of carbohydrates called FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) which can be difficult to digest for some people with IBS. High-FODMAP foods include wheat, onions, garlic, beans, lentils, and certain fruits like apples and pears.

2. Dairy products: Some people with IBS may have trouble digesting lactose, the sugar found in milk and other dairy products, which can cause gas, bloating, and diarrhea.
3. Gluten: Some people with IBS may have a gluten sensitivity or celiac disease, which can cause symptoms like abdominal pain, diarrhea, and constipation.
4. Fried or fatty foods: These foods can slow down digestion and trigger symptoms like bloating, gas, and diarrhea.
5. Caffeine and alcohol: These can cause stomach irritation and can trigger symptoms like stomach cramps and diarrhea.

6. Artificial sweeteners: Some artificial sweeteners can cause gas and bloating, which can trigger IBS symptoms.
It is important to keep a food diary, to track the foods that cause symptoms, and to avoid or limit those foods. Before making big changes to your diet, it's also important to talk to a healthcare professional.
The Ideal Diet for Managing Irritable Bowel Syndrome (IBS)
The best diet for IBS will vary from person to person as different foods can trigger symptoms for different individuals. But there are some general rules about what to eat that may help many people with IBS feel better.
Increase Fiber Intake: Eating a diet high in fiber can help regulate bowel movements and alleviate constipation. Good sources of fiber include fruits, vegetables, whole grains, and legumes.

2. Reduce Fructose and FODMAPs: Some people with IBS may be sensitive to certain types of carbohydrates called FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) found in foods like wheat, onions, and certain fruits. Limiting or avoiding these foods may help alleviate symptoms.
3. Avoid Trigger Foods: Keeping a food diary can help identify foods that trigger symptoms, and avoiding them can help alleviate symptoms. Common trigger foods include caffeine, alcohol, spicy foods, and foods high in fat.

4. Eat Small, Frequent Meals: Eating smaller, more frequent meals throughout the day can help regulate digestion and alleviate symptoms.
5. Consult with a Dietician: A dietician who is trained to work with IBS patients can help you create a personalized diet plan that takes into account your individual symptoms and triggers, and can also help you make sure that you get all the nutrients you need.
Management of IBS
The GI tract is an extremely complex system, influenced by many nerves and hormones. The type of food eaten, how often and where it is eaten, as well as some medications, all affect how the intestine moves and what it makes.
The most important part of treating IBS is figuring out how your symptoms are different from anyone else's and what might make them worse or start them. It's also helpful to know that it could take a while for bowel function to get back to normal and that symptoms could go away and then come back.
Dietary and Lifestyle Modifications
Regular, well-balanced, moderate-sized meals are better for the bowel than irregular, inconsistent meals. Allowing time for normal eating and restroom routines can ease IBS symptoms. Sleeping well and exercising moderately can lessen symptoms.
MSG and lipids may worsen symptoms for some. Some find that drinking a lot with meals worsens symptoms. Cooking veggies and fruits reduces IBS symptoms for some. If diarrhoea is the main sign of IBS, you should avoid coffee, cigarettes, and alcohol.
Your intestines may be more sensitive to gas if you have IBS. Limiting air and gas-causing meals can assist. Don't chew gum, gulp meals, drink carbonated drinks, wash down food with liquids, or sip hot drinks to limit air swallowed. Dentures that don't fit, postnasal drip, persistent pain, anxiety, and stress can increase air swallowing.
Low-FODMAP diets treat IBS. Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols are FODMAPs. The indigenous bacteria ferment poorly digested carbohydrates in the large intestine. Some IBS sufferers find that certain meals worsen their symptoms. For six to eight weeks, avoid particular meals to test the diet. If symptoms improve, introduce FODMAPs slowly in a safe amount. FODMAPs occur in many meals; therefore, avoiding them for a long time may increase your risk of nutritional deficiencies. The low-FODMAP diet helps some people, but we need further research to understand why. An easier low-FODMAP diet is available.

Note that IBS triggers vary by person. By keeping a food diary and writing down any bad reactions, you can quickly find and get rid of the foods that are giving you trouble and find a solution that works for you. Before permanently eliminating a food group, it is important to see a dietician who has advanced training in IBS, such as Maddie Lawson
Elimination diets prescribed by IBS-trained dieticians often fail. because everyone's IBS triggers are different. For comprehensive relief, a holistic approach must be taken.
Fibre
Plant-based dietary fibre, which the body cannot digest, helps manage IBS symptoms. Cooking food does not change its fibre content, although it may affect the gut. It's crucial to evaluate the fiber's volume and type (insoluble or soluble).
Increase your fibre and water consumption slowly. This reduces the risks of making a drastic diet change. Inulin (Benefibre®) or psyllium husk (Metamucil®) may be recommended by your doctor or nutritionist.
Insoluble fibres increase stool bulk, increase colonic muscle tone, and accelerate the transit time of gastrointestinal contents, thus relieving mild constipation.
Water-insoluble fibres include:
lignin (found in vegetables)
cellulose (found in whole grains)
hemicellulose (found in cereals and vegetables)
Soluble fibres form gels when mixed with water, making the bowel contents stickier and more resistant to flow (viscous), so that food stays in the digestive tract longer. This is important for people who suffer from diarrhoea.
Water-soluble fibres include:
pectins (e.g., apples, bananas, grapefruit, oranges, strawberries)
gums (e.g., cabbage, cauliflower, peas, potatoes, oats, barley, lentils, dried peas, beans)
It is important to note that for some IBS-D patients, a diet excessively high in bran fibre might trigger more frequent diarrhoea, while other types of fibre could still be helpful. Consult a physician or dietitian if you have any questions regarding the amount of fibre in your diet.
Stress
Gut nerves are independent (enteric nervous system). It controls digestion and waste removal. It interacts with the central nervous system. Stress, which can be caused by not getting enough sleep, working too hard, or consuming too much caffeine, alcohol, or cigarette smoke, is common among IBS patients. Stress, despair, panic, and worry can exacerbate IBS symptoms. Rest and exercise lessen stress and IBS symptoms.
Psychological therapy, which includes learning to relax, manage time, adjust your lifestyle, or think differently, can aid medical treatment.

Physiotherapy/Osteopathy
Pelvic floor muscles regulate defecation. IBS patients may have pelvic floor incoordination (dyssynergia or anismus). A physiotherapist/osteopath for pelvic floor rehabilitation may do a physical vaginal exam on a woman, a rectal exam, an EMG biofeedback exam, and observation and palpation of the perineum and abdominal wall. Physiotherapy and osteopathy can assist patients in learning to relax the pelvic floor and allow the deep abdominal muscles to push the bowel completely. Physiotherapy may help people with diarrhoea and urgent, watery stools. Find an experienced incontinence or pelvic floor physiotherapist through your regional physiotherapy organisation.

Medications
Medication to normalise bowel contractions helps many IBS patients.
Some products add bulk to stools to help the intestine control transit time and stool composition, relieving diarrhoea and constipation. These bind water and loosen stools.
Other drugs may reduce symptoms in different ways. Pancreatic enzymes may help some IBS patients digest better. Bile salt binders like cholestyramine prevent diarrhoea, especially in the fast-moving small intestines. Low doses of antidepressants and anti-anxiety drugs may calm the nervous system in the gut, reduce pain, and help you sleep. Plant-based Iberogast® may reduce IBS symptoms. These drugs vary in efficacy.
Stimulant laxatives speed up digestion by contracting muscles. They can relieve constipation but also potentially cause stomach cramps, pain, or discomfort, diarrhoea, electrolyte imbalances (including low potassium), and nausea. Therefore, only use stimulants temporarily.
Antibiotics
Rifaximin is an antibiotic that is approved to treat IBS-D symptoms in adults. It is a 14-day treatment that helps relieve IBS-D symptoms like stomach pain, bloating, feeling like you have to go to the bathroom right away, and diarrhoea. It isn't absorbed very well, so it only works in the gut. It might work by reducing bacteria and bacterial toxins in the digestive tract. It can also help ease other gut symptoms that aren't caused by IBS by reducing inflammation in the gut.
Probiotics
When taken in the right amount, probiotics, which are mostly bacteria and yeasts, are good for your gut. Microbiome disruptions or improper microorganism interactions may cause chronic gut disorders. Scientists are now looking for new ways to change the complex environment of the intestines to treat microbes that are hurt by drugs. They have also pushed doctors to minimise antibiotic use. Some antibiotics assist with IBS.

IBS treatment with probiotics has many drawbacks. Many commercial goods have less live bacteria than advertised. Most probiotics added to meals like yoghurt are killed by stomach acids before they reach the colon, where they need to be alive to work. As marketers promise, yoghurt may not contain enough microorganisms to benefit intestinal health.
Many commercial products include enough probiotics and are formulated to survive an acidic stomach. New research reveals that specific probiotics work only for certain medical disorders. Make sure your probiotic can address your medical issue.
Probiotics' effects on GI health are still being studied, but this fascinating field is moving fast. Align® (containing Bifidobacterium infantis 35624) treats abdominal discomfort, gas, and bloating, and Bio-K+® IBS Control (containing Lactobacillus acidophilus CL1285®, LBC80R®, and CLR2®) improves quality of life in diarrhea-predominant irritable bowel syndrome (IBS-D) patients.
Florastor® contains Saccharomyces boulardii lyo, a digestive yeast found on lychees and mangosteens. This yeast controls stool frequency and regularity. BioGaia® ProTectis® Drops with Lactobacillus reuteri reduce colic in infants.
Common IBS mistakes to avoid
There are several common mistakes that people make when trying to manage their IBS symptoms on their own:
Not keeping a food diary: Keeping a food diary can help to identify specific foods that may be triggering symptoms. Without this information, it can be difficult to make dietary changes that will effectively manage symptoms.
Making drastic dietary changes: Cutting out entire food groups or making drastic changes to one's diet can lead to nutrient deficiencies and an unbalanced diet. A trained dietitian can help to make dietary changes that are both effective and sustainable.
Self-diagnosis: IBS is a complex condition with a wide range of symptoms. Self-diagnosis can lead to misdiagnosis and delay in getting appropriate treatment. It's important to see a healthcare professional for proper diagnosis.
Not addressing underlying psychological issues: IBS can be linked to stress and psychological issues, such as anxiety and depression. Not addressing these underlying issues can make it difficult to effectively manage IBS symptoms.
Not seeking professional help: IBS can be a complex and difficult condition to manage. Seeking the help of a healthcare professional, such as a gastroenterologist or a dietitian, can greatly improve the chances of finding an effective treatment.
What to do to stop IBS
Because nutrition can help manage IBS symptoms, working with an IBS-trained dietician is crucial. A dietitian can figure out what foods might be causing symptoms and make a personalised eating plan that relieves symptoms while still giving the person a healthy, varied diet.
Our dietician at the health collective can teach IBS patients how to increase fibre, minimise fat, and follow a low FODMAP diet. We can also give advice on how to avoid nutritional deficiencies caused by food limitations. IBS patients can live a normal, healthy life with the support of an IBS-trained nutritionist.
Our skilled IBS dietician can help you figure out what foods set off your symptoms and get rid of them, make a custom diet plan for you, and balance your diet so you get all the nutrients you need.
Leave IBS behind. Take charge of your health and your life. You can get rid of IBS symptoms and live your best life if you get the right care and support. Don't let IBS control your life any longer.
Book a consultation with our highly-qualified dietitian at our clinic now. Our team will create a customized nutrition plan tailored to your specific needs and help you achieve your health goals. Schedule your appointment today and take control of your well-being!
CLAIM YOUR $50 VOUCHER AT THE HEALTH COLLECTIVE
Fill out the form below
For New patients to The Health Collective only.
One voucher per person for select services including Chinese Medicine, Acupuncture, Dietetics, Nutrition, Massage.

 DAMIAN POUSTIE Poustie
DAMIAN POUSTIE Poustie